University of Liverpool – Directorate of Nursing Prize Giving 2018
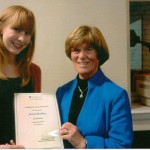
The Rebecca Haynes Award 2017. Charlotte Williams
My experiences since qualifying
I graduated from the University of Liverpool on the 6th December 2017. Shortly after, I started working in the Royal Liverpool University Hospital. I am based on the Emergency Surgical Assessment Unit (ESAU) but will soon be moving to the Accident and Emergency (A&E) department and the Acute Medical Assessment Unit (AMAU) as part of my year rotation around the emergency floor.
Becoming a qualified nurse has been the most challenging but rewarding thing I have done to date. I have just started to adapt to the long hours and tiring shift patterns and am slowly embracing the level of responsibility a registered nurse undertakes. I have seen so many new things since starting and have been faced with various situations and circumstances that have challenged me emotionally, ethically and physically. As a result, I have developed and am continuing to develop myself as a competent nurse. The level of support I have received since qualifying has been tremendous; I have been able to comfortably ask questions and have received lots of advice from senior members of staff. In response to this, my confidence is growing. I am enjoying every shift more and more as I begin to feel more capable. It truly is a pleasure and an honour to do what I do. I have the opportunity to make a difference in the lives of so many people. I have also been involved in the education of future nurses; I have had a few students working with me which has allowed me to pass on my knowledge and shape the future of nursing ever so slightly. I am extremely excited for what is to come, individually and also for healthcare as a whole. My plans for the next year are to finish this rotation and to be a part of the new Royal Liverpool University Hospital when it opens later this year.
University of Liverpool – Directorate of Nursing Prize Giving 2017
On 6th December 2017 3 Nurses’ League committee members attended the prize giving for the nurses who were graduating at the end of their BN (Hons) Degree course.
We were pleased to be able to present the Rebecca Haynes Award for the highest marks achieved at the end of the final year to Charlotte Williams. Charlotte is now employed at the Royal Liverpool Hospital on the 12 months Emergency Rotation Scheme and is spending the first 6 months on the Emergency Surgical Admissions Unit. For the following 6 months she will work in either the Acute Medical Admissions Unit or the Accident & Emergency Department and can then decide which area she prefers to continue to work in on completion of the scheme. She will be telling us more about her experiences in the 2018 newsletter.
The Laura Jones Award for the highest marks achieved in the first year went to Emma Taylor, who unfortunately could not be there on the day to receive her certificate.
Each of the 2 students receives £100 to help further their nurse education.
40 students graduated on this occasion, and we were privileged to present each of them with their Liverpool University School of Nursing badge. We wish them all every success in their future careers.
Carolyn Rankine (League President)

Charlotte Williams receiving the Rebecca Haynes Award with Carolyn, Margaret & Sue
WINNERS FOR 2016
Carolyn Rankine and Jane Kemp attended the prize giving of the 2016 graduans at Liverpool University yesterdayHere are Rachel Jackson and Rebecca Turner, joint winners of the Mary Jones Award . Their marks were identical for their assessments during their first year of training, so both were worthy winners.

Rachel Jackson & Rebacca Turner. Winners of Mary Jones Award
Rachel is at present working on the Vascular Unit at RLH and Rebecca is on the Cystic Fibrosis ward at the Heart & Chest Hospital. Both girls are enjoying their placements and looking forward to having Chrismas off this year.
This is Lorna Brooks, the winner of the Rebecca Haynes Award for the highest marks in the final examinations.

Lorna Brooks. Winner of Rebecca Haynes Award
Coincidentally Lorna was also winner of the Mary Jones Award after her first year.
She has just completed the first month of her new job on a cardiac surgical ward at the Heart & Chest Hospital and is enjoying the challenge of a new career with the Trust.
WINNERS OF THE MARY JONES AWARD 2015
WINNER OF THE REBECCA HAYNES AWARD 2015
Rebecca Haynes award to Emily Chesterman. Please click on the link to read Emilys response to receiving the award.
WINNER OF THE KATE MORLE PRIZE IS LAURA ROWLAND
Unfortunately we do not have a photo of Laura currently.
AWARD WINNERS 2012
On 12th December 2012 Carolyn Rankine and I attended the post graduation ceremony at the Whelan Building for the BN (Hons) Graduates. As you can imagine it was a very happy and lively gathering of graduates with their families and friends enjoying their success.
We met Julie Crane again who is the new Head of Department of Nursing Studies. We had both worked with her in earlier times so it was good to meet up again and create links for the future.
Lucy Mead won the Mary Jones Award for achieving the highest mark at the end of the first year. Unfortunately she was unable to be there on the day so I don’t have a photo to share.
The 2nd year Kate Morle Award was given for the first time to Connie Brown for excellence in clinical practice. She has promised to give us more information on her research on homelessness with the YMCA and I will post it when received.
Helen Pennington won the Rebecca Haynes Award for achieving the highest mark at the end of the final year. 
We then presented the group with their Badges and stayed for a while talking to everyone. It came as a surprise that some thought the awards were a University prize and were not aware of the old LRI building. So we can raise our profile a little I think and perhaps get them to look at our website to see the olden days! It was a lovely occasion and I felt very privileged to be there. It was so nice to see the enthusiasm and energy in this young group of people upon starting their careers.
2011
On December 15th 2011, three members of the Nurses` League Executive Committee were invited to the post graduation get together in the School of Health Sciences when the 2011 Nurse graduates received their University School of Nursing badges.
Presentations were also made to the two recipients of the 2011 Liverpool Royal Infirmary Nurses` League Awards, Carol Paisley and Jessica Bradbury.
Jessica Bradbury, the recipient of the Mary Jones Award 2011 (best 1st year nurse) receiving her certificate from Ann Spencer.

Carol Paisley, recipient of the Rebecca Haynes award (best final year student) receives her certificate from League President Ann Spencer.
WINNER OF THE MARY JONES AWARD 2008. JOINT WINNER SAMANTHA HARRISON.
After completing my A Levels at college, I began work in a local nursing home in order to gain experience in health care and to ensure that nursing would be the right career choice for me. During my second year of working at the home I was certain that I wanted to apply to study nursing, as I had thoroughly enjoyed my work there and felt ready to further myself in this area.
My first year at the University Of Liverpool has been challenging both academically and practically, but I have enjoyed every part of it which has further motivated me to pursue a career as a nurse.
So far, I have been given the opportunity to work at Arrowe Park, Whiston and the Royal Liverpool Hospital, on nephrology, orthopaedic, elderly care and urology wards. I don’t have a favourite placement, as each one has given me different opportunities and experiences, which have been invaluable to my learning and I look forward to my future placements.
I am undecided as to which area of nursing I would like to work in when I qualify. I want to keep an open mind and to continue to enjoy my training and see where it takes me.
WINNER OF THE MARY JONES AWARD 2008. JOINT WINNER DANIEL WILSON
After leaving school with good A Level grades, I spent over 10 years working with residential mental health teams. I started as a volunteer in a hostel for the homeless, then spent some time working for Merseyside Probation Service. I moved to London, where I worked as team manager for a charity which helped offenders with mental health problems. After a few years as manager, I decided to change my career, retrain and relocate back to Liverpool, where I was born.
I had always wanted to be a nurse, so I made the decision to go in a new direction and apply to study adult nursing. I am 38 years old, taking the plunge and radically changing my life, wasn’t easy. I had lots of doubts about making this change, but doing so has proven to be correct and I couldn’t be happier with my training or my university.
My first year was a real challenge, having never worked on a ward before. I was on placement at Broadgreen, Arrowe Park, Whiston and the Royal Liverpool Hospitals gaining experience on orthopaedic, urology, respiratory and elderly care wards.
My favourite and most successful placement was in care for the elderly, where I found I had a real skill in working with older patients. I am now considering this as my chosen speciality when I qualify in 2010.
Daniel Wilson. February 2009
WINNER OF THE REBECCA HAYNES AWARD 2008. JOINT WINNER LAURA CURRAN
It is incredible to think that it is over three and a half years ago that I moved to Liverpool from Shropshire, to begin my nurse training. Looking back, although my training was greatly enjoyable, it was also full of long hours, tiredness and a great difficulty in juggling academic work, practical training and a ‘normal’ life. However now, as a qualified nurse, those challenging times as a student seem insignificant and I can see that the means really do justify the end. Having been fortunate to obtain the Mary Jones Award at the end of my first year of training, I now feel very honoured to have been awarded the Rebecca Haynes Award at the end of my training.
I send a big thank you to my friends, family and to those I trained with, for their help and support throughout.
Following completion of my course in September 2008, I began applying for a post in Liverpool, a city I am very happy in. I was lucky enough to be offered the second post I applied for, at the Liverpool Heart and Chest Hospital, working on a ward specialising in the care of patients who have undergone cardiothoracic surgery. Having never envisaged myself doing this sort of nursing, I was pleasantly surprised to find that I love it.
I remember being absolutely terrified the day I first wore my blue uniform, even ironing it twice to make sure I looked my best. Similar fear struck me the first time I did a medication round on my own and when I began my first set of night duty, things that are now second nature to me.
With regards to my training at the University of Liverpool, there is probably not a day that goes by that I do not utilise some part of my nursing studies. My training allowed me to work in a number of different areas and Trusts across Liverpool, enabling me to draw on good practices I had experienced in a variety of settings.
It saddens me to hear modern nurses being criticized for not being as caring as nurses in previous times. My training taught me to be compassionate, understanding and defend what is known to be right, in the name of excellence in patient care. At work I find myself surrounded by talented and extremely caring nursing staff and as testament to their work, I find myself thinking, ‘how could it have ever been better’? I do agree that the current situation is far from perfect. Most commonly, my peers are troubled by lack of nursing staff on the ground, which often leads to less time to care for patients and therefore much distress and stress for nurses. With this in mind, I welcome new initiatives such as the ’productive ward’ which aims to ‘release time to care’ by streamlining the work we do that does not involve direct patient care. I hope that projects such as this find success, so that nurses do not suffer from burn out, allowing them to enjoy what really is a wonderful vocation.
Laura Curran. May 2009
WINNER OF THE REBECCA HAYNES AWARD 2007. CRAIG SIMON
Since being awarded the Mary Jones award in December 2004, I have been fortunate to obtain a first class degree with honours. I have also been awarded the Rebecca Haynes award and I am extremely honoured to be the recipient of both awards during my nurse training. Upon completion of my training and registration with the NMC I have commenced employment with the Haematology Unit at the Royal Liverpool University Hospital. I am very fortunate to have obtained this role which I have sought after since my second year placement on the Unit. I particularly enjoy the diversity of such nursing, and although emotionally draining at times, the relationship built with our patient group makes the job an extremely rewarding one. It shocks me to see the changes that have occurred within nursing since winning the Mary Jones award. I remember commenting on the scope of opportunities available within nursing, yet the most prominent change is the lack of vacancies for fellow graduates and students due to graduate. It saddens me to see many great nurses either unemployed or in employment unconnected to nursing. I can only hope, along with those affected, that the situation improves and it doesn’t deter people from entering such a great profession.
That said the future of nursing and the role of a nurse appears due for radical change. Policy aims to push further services into the community and away from the hospital setting. I feel as a profession this change should be embraced and viewed as an exciting time for nursing. Yet with such changes I hope the history and uniqueness of our role is not lost. I feel it is up to nurses to continue to view and care for patients as people, rather than turning them into a condition, statistic or objects to meet health targets. I hope that my future can bring as much success as my training has. My decision to change from medical to nursing student has been one of the most significant and rewarding I have made. My ambitions for the future include further academic study in the form of a Phd. and career advancement to hopefully a specialist role within haematology/oncology nursing. My overriding aim for the future is to continue to provide nursing care to the absolute best of my ability and hope that as a result I can be a part of shaping the future of our profession.
Craig Simon April 2007
MARY JONES AWARD 2006 Laura Curran
Unlike many nursing staff and students around me I didn’t always know that I wanted to go into nursing. The idea only began to grow on me whilst I was studying for my A-Levels but despite this, for me now, nursing is a vocation. I moved to Liverpool around 18 months ago and I have found the city a great place to study, work and live. The course can, at times, be very physically and emotionally challenging and I am still learning how to meet deadlines without the last minute rush. However, this is more than balanced by the fun and rewarding times that the course can bring. There can be much discrimination and inequality in the world but by its nature nursing practice treats people with respect and understanding. I have had the pleasure of working with many student and qualified nurses who strive to recognise the individuality of each patient, helping them to access the quality health care and support that they need. So far I have particularly enjoyed my hospital based placements on respiratory and gastroenterology wards. My current placement in the community setting has really opened my eyes to the wealth of extended roles and services offered by nurses. I am looking forward to experiencing new areas of nursing care and I am unsure about my future plans, but a community role would definitely be something I would love to do.
Laura Curran
WINNER OF THE REBECCA HAYNES AWARD 2005 . HANNAH THEWLES.
Hannah has sent us this information about herself. I spent three years studying for my nursing degree at Liverpool University. The course was not an easy one, but it was extremely rewarding. The academic standard expected was high and was combined with working shifts which could be physically demanding and emotionally draining. While sometimes tough, working on the wards was also fun and a fantastic opportunity to observe some truly inspirational nurses. In the second and third years of the course we had more freedom to pursue subjects that fascinated us in greater detail. Whilst not always appreciating rapidly approaching deadlines, I loved the challenge and stimulation of the material we studied. Implementing and expanding that material on the wards provided a good basis for practical nursing skills. Having enjoyed the course so much, it was a real honour to receive the Rebecca Haynes award at my graduation ceremony.
Following the end of my degree I married and moved to Birmingham where my husband is based. The skills I acquired both academically and practically have proved invaluable to me as I have commenced my nursing career. I am currently working in the Cancer Centre at the Queen Elizabeth Hospital. Nothing can prepare you fully for the transition from student to staff nurse (and the shock of being assigned your own students!), but having survived the first few months, I am thoroughly enjoying myself. In the future I would like to move into a palliative care setting which is an area that particularly interests me. The opportunities that are available within nursing are one of the many things which make it such an exciting and varied career.
WINNER OF THE MARY JONES AWARD 2005. KIRSTY NUTTALL.
Kirsty has written to tell us a little about herself and what the award means to her.
Many of the nurses known to me, both qualified and students alike tell me of how they have always wanted to become nurses, however, this bears little resemblance of how I have come to be where I am today. Whilst studying for my A levels I was faced with the challenge of deciding which path to take for my future, and all I knew was that I wanted to make a difference in the world. After careful consideration, I firmly believed that nursing was what life held for me, and almost a year and a half on, although not making world changing differences (yet), nursing has become a part of who I am. The Bachelor of Nursing programme has been and continues to be one of the most challenging experiences of my life and yet the most enjoyable, and although sometimes difficult to juggle placements with assignments, the real differences I am making in people’s lives makes all the hard work worthwhile.
As for the future, I am not sure what it holds, but I do know that nursing is where I want to be. I am delighted and proud to have received the Mary Jones Award and cannot give enough thanks to all those who continue to encourage and support me, including family, friends, staff and patients. Thank you.
NURSES LEAGUE TRAVEL AWARD WINNERS
2000 Tom Donovan
2002 Elizabeth Cooper and Victoria Garner
2005 Sue Redfern
2007 Sarah Doyle
2011 Christine O’Connor. Becci Sloane & Abigail Hosier
2013 Jenny Wharton
2015 Not awarded
2016 James Ridley
Travel award Accounts
Amanda Wood
Nurse league travel award 2017- Visit to University of Malaya and University of Malaya Medical Centre. Kuala Lumpur. Malaysia.
I have been working as a research nurse for the University of Liverpool for the past 9 years recruiting patients for many orthopaedic based studies. As my manager Professor Simon Frostick has academic links with the University of Malaya we applied and were successful in a bid for a Newton grant funded project. This was a yearlong study looking at the vulnerability of older people in Malaysia to urbanisation and climate change. Newton grants main aims are to develop science and innovation partnerships that promote economic development and welfare. We were unable to find any research nurses or nurses with any research experience to undertake the study and so the team consisted of a business manager with pharmacology experience and 2 retired very experience nurses and student doctors. Therefore, they all needed training in carrying out a research study to a high standard. I was responsible for training the study team in how to obtain research consent taking into account ethical and governance issues.
As we also have dual PhD students from Malaysia who have no access to research nurses when in Malaysia and so part of their valuable study time is taken up with the practicalities of collecting research specimens and collecting data from clinical teams with no research nurse to act as an intermediary. I therefore applied for the nurses travel award to visit the University of Malaya and the medical centre to promote building the role of the research nurse.
Prior to arriving I set up as many meeting as possible with key stakeholders within the University and the hospital the university of Malaya medical centre (UMMC). Before I left I spoke to the International Association of Clinical Research Nurse (IACRN) to gain any insights into promoting research nursing internationally. They advised me that clinical research roles in the UK has increased rapidly due to government directives and the drive for evidence based medicine. NIHR nurses provide the majority of recruitment as they support research from commercial companies. Involving nurses has increased recruitment whilst ensuring high quality data and research. They suggested finding out about what research was currently being undertaken and what obstacles they had and the current nurses involvement in research.
I firstly met with the department of nursing services Associate Prof. Dr. Khatijah Lim Abdullah in the University of Malaya. Currently the University has a 2-tier system for nurse training 20% degree nursing and 80% diploma nursing. The plan is to encourage more degree nurses. The diploma nurses have very little in the way of formal research education whilst the degree nurses have some taught evidence based medicine and a small research project at the end of the course and they are encouraged to publish their finding but only a small percentage make this jump.
Nurses once qualified in Ministry of Health (MOH) hospital have to stay in the post graduate job assigned to them for 5 years they are not allowed to move and have no say in the assignment. They must pay an exit fee to leave which most nurses cannot afford. The Malaysian nursing boards director is a doctor and not a nurse, the nursing board is a sub division of MOH and not an independent body.
The main stumbling block to nurses advancing their roles is that the Nurses act 1950 has never been updated. Within the act nurses cannot consent patients even with principle investigator delegation and so nurses cannot make this leap in their practice. Prof Khatijah Lim Abdullah and her team have been trying for the past 5 years to get the act updated to reflect the modernisation of nursing practice and are hoping with their continued pressure changes can be made soon.
The Department is also involved in research, in order to meet the emerging needs of the country. The Nursing Research Steering Group (NRSG) was initiated by the department staff and nurse educators from the College of Nursing, University Malaya Medical Centre (UMMC) with the vision to be a pioneer in nursing research activities within the UM and UMMC. NRSG recognizes that nursing needs to be transformed into a research active profession.
Nurses steering group University of Malaya
I had the pleasure of going to the ministry of health in Putra Jaya, Kuala Lumpur and met with the Principal Assistant Director of Nursing, Gowry Narayanan. Her main role was writing and regularly updating the standard operation procedures for all nursing practice with her team of staff. She said that the Ministry of Health nursing focus is now on falls prevention and pressure ulcer prevention in hospital stay patients. They have developed specialised teams to focus on these areas which do include some nurses but they are managed and led by doctors. She reiterated that as the nurses act prevents nurses acting autonomously on many levels the advancement has not happened within the profession but that hopefully with more degree nurses going through training there will be a change in the future. The focus of research sits very much with the medical profession and nurses only assist in the study data collection and she could not see this changing in the near future.
Each university hospital in Malaysia has a clinical investigation centre (CIC). I met with the head of the department Prof Hasniza and her experienced research team. It is a well-equipped purpose-built unit for carrying out pharmaceutical clinical trials and has several commercial sponsors. They have become very successful and have won many awards for their high standard of drug trials. Here the doctor will recruit the patient and consent the patients whilst the nurses will carry out the study assessments and data collection. I found here that nurses have managed to develop their role to become study co-ordinators and the successful nurses are highly sought after by the clinicians to assist in complex studies. I spoke to the research nurses in the team and they all seemed happy with their role and stated they would be reluctant to take on extra duties in place of the doctor such as recruitment and consent as they felt that was the doctors role especially as they were drug trials. They all undertake appropriate training for the role, medicine training and good clinical practice and were excited to be involved in research.
I also met the with UMMC Chief Nursing Officer Madam Yasin Abidah and her team of Matrons in the hospital. They all work hard at promoting a high standard of nursing care in the hospital but admitted that nursing is very much task orientated still. They have issues with staff retention as many nurses leave after the compulsory 5 years for jobs abroad such as Australia and Singapore for improved pay and advancement in careers. They have no advanced practice roles for nurses and they felt the only advancement nurses can make at the moment is the progression to management level. They do have some teams that include nurses looking to improve areas such as falls management but that it is Doctors that prescribe all care which nurses must follow with little allowance for nurses using their own critical thinking skills.
After my many visits to Malaysia this was a very enlightening trip which highlighted the current issues with nurses advancing their own roles and careers. There are many socio-cultural factors that limit the development of the profession. The majority of nurses are women in Malaysia and only a small percentage are men, however this has been growing over recent years. Together the status of women, fuelled by the powerful forces of both tradition and cultural values, serve to ensure that much remains to be done to improve the status of nursing. With increasing numbers of degree nurses and equitable access to post graduate education there will hopefully be a sea change where nurses can find their voice and push for a transformation of the nurses act and ultimately their own advancement. This could then lead on to nurses being more actively involved in research. I would really like to go back again in the future and see if I can help to improve nurses involvement in research through training and development which in turn could help them overcome the obstacles they currently face.
University Malaya Medical Centre
2016 Nurses Travel Award winner
James Ridley
SAAHAS, INDIA
25TH MARCH – 7TH APRIL 2017 JAMES RIDLEY
Uttar Pradesh;
To understand the reason for this visit then I feel that you need to understand the country and the region, something that fascinated me before I arrived, held my fascination whilst I was there and continues to offer me a sense of questioning since my return.
My visit to India was based within the state of Uttar Pradesh (UP), this is a state within the North West of the country and is identified as an important border state as it connects with Nepal. According to the official website for this state it equates to almost 2.5million square kilometres, to give context this means that this single state is half the size of France, 3x the size of Portugal, 4x the size of Ireland, and a little bigger than England, this state is the fourth largest area within India, (www.up.gov.in). In relation to population then UP is also identified as the most populated state within India, this state has seen significant increases in its population, 548 people per square kilometres were recorded in 1991, however this has increased to 828 in 2011, nationally this represents 16.17% of the entire Indian population.
The state is dominated by rural communities, however there are a number of cities (Moradabad, Rampur, there are more), towns and villages, the state capital is Lucknow which is south of the area where I was staying. The state is broken up into districts as can be seen by the map provided on the front cover, I was based within the district of Moradabad. In terms of travel my place of visit was 7 hours drive from New Delhi, and was surrounded by farming communities. I was based in Billaspur
and the nearest main city was 2.5hrs away in Moradabad, based on United Kingdom roads and infrastructure this would be an easy route, however infrastructure and connections to cities, towns, and villages is poorly managed. The location and distance from New Delhi means that this area doesn’t bene t from the infra-structure of a large city area, or even a large town. Roads are crumbling, medical practitioners are scarce or based within larger towns, and the main employment here for families living within the villages is daily farm labour. The main source of employment is farming with 65.9% of those working based on farms. The farms local to my base produced sugar cane, rice, and wheat, which was mainly harvested by hand. It was explained to me that farm workers can expect to receive anything from between 300-500 rupees per day (approximately £5-7 per day) however work is not guaranteed every day. Employment within this state is 23.7%, less than a quarter of the population, and for some there may be only a single person working and providing for their entire family.
SAAHAS;
The journey that has eventually enabled me to travel to India began 3yrs ago, it started with a simple social media posting about a program called “SAAHAS”. This program was developed to seek out people with an intellectual disability and support them to gain access to health, welfare and support which is similar to the role of learning disability services within the UK.
This program identified that people with an intellectual disability were “invisible” to services and statutory provision within the rural areas of Uttar Pradesh. How does this related to nursing practice? As a learning disability nurse our role is to lead the way in achieving positive health outcomes for people with learning disabilities. We will use an inclusive and collaborative approach to address barriers to social inclusion
and will function as integral members of the wider family of nursing, developing and using specialist knowledge and skills to improve health and well-being of children, adults and older people with learning disabilities across all settings.
The main difference here is that it is completely managed as an initiative within the UP (Uttar Pradesh) state police service, and is led by a senior member of their police service. The founder of this program was a man called Rahul Kumar, his rank within the service is a Deputy Superintendent of Police (DSP). His motives for beginning this program was based on his role as a police officer, which means that he is responsible for managing crime and fundamentally crime prevention. Making the “Invisible – Visible” is a theme to this program and certainly has led a number of the initiatives that I observed and hopefully contributed to. Valuing People (2001) identified within the UK that the role of public services is to ensure that no matter how complex a person’s disability that they are enabled to live full and equal lives in their local communities. It’s with that in mind that I wanted to meet and see how SAAHAS was engaging with people who have an intellectual disability and their families, and how the role of the police can support the principles that I am familiar with within my nursing role.
UK;
In the UK it has been difficult to identify a definite number of how many people with learning disabilities live within the UK. It is suggested that there are approximately 1.14million people with learning disabilities living within the UK; 236,000 children, 908,000 adults aged 18+, of whom 199,000 (22%) are known to GPs as people with learning disabilities. (Emerson et al (2013)
India;
Indian census completed in 2001 identified that about 2.13% (21 million people) had a disability, (Indian Government, 2003). National Sample Survey Organisation (NSSO, 2003) suggested that the figure for people with a disability was 1.8%. The NSSO figures suggested that 75% of their figures were individuals living within “Rural Communities”. Survey included recognising the following as a disability, visual, hearing, speech, locomotor, and intellectual disability, (Chavan & Rozatkar, 2014). However Ganesh et al (2008) identified that they felt that numbers of people with ID was much greater.
I highlight the points here due to the similarity related to identifying those individuals within our communities (UK and India) who have an intellectual disability. There is statutory provision offered to people with an intellectual disability in the form of health, education and welfare, however accessing this is based on identification and certification. Within the UK this process is in the main more streamlined as children, and their families will likely have input from a range of health professionals, health visitors, child development centres and at the required age then some access to education. This is also likely to be backed up with a range of information, family support groups and discussion which can be accessed to support families to identify what they are entitled too.
Identifying individuals with an intellectual disability is one of the main functions of the SAAHAS program as without formal assessment and certification then individuals and their families cannot access the services to which they are entitled too. In the area where I was based the biggest issue was access. Within UP there are identified as 97,184 inhabited villages which is the main area identified as “rural”. Accessing these villages as I found out was at times extreme, there was little if any infrastructure other than the village leaders, no public transport, and for many villages a long drive or significant cant walk to the main highway. Reaching the main highway enable access to some forms of transport, and then a further long journey was likely for individuals and their families to enable access to a town/city which had practitioners who would be able to certify their family member as having a need which would entitle them to state/ national provisions.
Disability Certification
This is Shaleema and Faroum, brother and sister, they lived in a village which was well established. They live with their large extended family, which is seen as a bene t to the family both financially and in terms of support. Their father is a farm labourer, and on the day of my visit he had been to collect his day’s wages (300-500 rupees), which equated to approximately £5-7 per day. This family had been recently identified by the local constable as having members with an intellectual disability. This constable, who as part of the SAAHAS program is tasked with speaking to village leaders and families about residents within the village. I was told that they would stay within the confines of the family compound whilst other members completed work or other chores, however what was significant was that I was informed that the position of the family’s home created an increased risk to Shaleema
 Shaleema and Faroum
Shaleema and Faroum
and Faroum. They lived on the outer rim of the village and the house was surrounded by fields, I was told that this increased the risk of them being taken whilst unsupervised and this was a genuine concern for the family and the officers who were visiting with me.
Shaleema and Faroum’s family informed me that they had other siblings but they were the middle children, their siblings were married and didn’t live in the village. They were not registered with the local services, they weren’t certified as having a disability, and therefore they weren’t entitled to state welfare provisions. On the day of this visit I was informed that this was a new village to have been identified and that there was a plan for the SAAHAS team to provide transport for all families to enable them to access the local certification services and therefore entitle them to welfare provision. I was informed that the most important aspect of this would likely be the “pension”, this equated to 300-500 rupees per month for each individual who was identified as having a disability, the rate depended on the certified level of disability. I asked whether this would have a big impact on this family, I was told that this would be a significant amount of money for a family such as this and would offer not only financial aid but also some security to the family. This family were not aware of the financial support that they were entitled too, they were also 1.5hrs drive away from the main highway and then a further 1-2hrs away from the town which would enable them to see a practitioner who would complete the

Getting to Know you , Garou
certification paperwork. SAAHAS offered this family transport, assistance and on the day of my visit completed a “Health Passport” which I had brought from the UK to enable the family and the certifying practitioner to see more information about who these individuals were and what their needs were. Offering families and individuals access to support and welfare systems not only enables those families to gain financially it also enables local services to have a more accurate idea of who they are required to support within their region.
This little boy is Garou, he lives in the same village but has different needs. He is 9 yrs old, his family informed me that he has had epilepsy since he was 6months old, and this followed an accident where he fell out of his cot. His family have access to a Neurologist for Garou and he is prescribed medication to manage his epilepsy, however he wasn’t registered with a school, or accessing the welfare systems available to his family.
Health Passport
During my visit I was asked if I would complete sessions for local “ASHA” (Accredited Social Health Activist) workers and local primary school teachers about the needs of people with an intellectual disability. The role of the ASHA worker is part of India’s response to health concerns within rural communities (Government of India, 2005), however they can be expected to also outline other health related programs, (Shrivastava & Shrivastava, 2009). In India there is an acknowledgement that approximately 70% of rural child related deaths can be attributed to poor access or delayed access to health care services, with the majority of deaths for the under 5’s being related to conditions which have existing interventions, (Mahyavanshi, et al, 2011). This is an important group of workers as they are familiar to villagers, and in some circumstances may actually be from the village or a village close by. Offering these workers some insight into the aetiology of intellectual disability was seen as a way of helping them to support families and identify children at a much younger age (under 5) who may have missed some of the developmental milestones. As part of the role of the ASHA worker is to support maternal health and the health of the child then it was important to share information related to factors which may lead to a child having an intellectual disability such as maternal health, nutrition, and prevention of disease and illness which may lead to infection.
ASHA Workers
Early intervention for families in the UK is seen as a major support for parents and their children to access the support services available, but can also support the emotional transition that comes with having a child with an intellectual disability. Having ASHA workers understanding some of the needs of people with an intellectual disability may enable them to speak with parents about minimizing some of the risk factors; however, identifying the health needs of people with an intellectual disability will also enable the ASHA worker and the family to hopefully signpost to other health interventions and register them with local services.
Access to education has become a right for all with a disability within India since the passing of law (Persons with Disabilities (Equal Opportunities, Protection of Rights & Full Participation) Act, 1995). However, even with there being a legislative framework for children and young people to access education there continues to be the same issue of whether a child is registered, if not then schools will not be aware of those children and they won’t be given access to education as identified by Limaye, (2016). In a similar rationale to the work of the ASHA workers I met and spent time discussing the needs of children with an intellectual disability to primary school teachers. Offering some education and training in relation to supporting people with an intellectual disability was the focus of the session, however as identified by Mondal and Mete (Date Unknown) teachers require more specific training and learning to enable them to understand the needs of children with an intellectual disability. I was told of a family who had a daughter who was able to access education within an integrated school, however their child was excluded from the school due to her behavior. The child’s behavior was “spitting” and this was found to extremely distressing to the school staff and was an excluding factor for the child in relation to their class mates. I discussed with the person involved about whether anyone had considered why the child was using that behavior and offered some insight into reasons why that type of behavior may be used. It was clear to me that had someone considered some of the supportive aspects of communication, person centred care and simple behavioural assessment then some greater insight could have been gained. However, the teaching staff were given no skills to enable them to complete this and therefore they felt unable to support this child.
 Speaking with Primary Teacher
Speaking with Primary Teacher
I was fortunate to visit the “Special School” which had recently been opened by SAAHAS for children who were living in the area just outside Moradabad. I met with families, their children and the teacher who I was informed didn’t have a formal teaching qualification but had completed training in vocational training for people with intellectual disability.
This is the only special school within the area and was opened in 2016, as with all of the other projects SAAHAS has been involved in it started slowly with many parents not being able to access transport to the school which for some is an hour away or be able to leave other family members. This building is a former hostel, it was never a school but what it has become is a place where children and their families can share ideas, learning and acceptance. One of the projects coming into the school whilst I was there was enabling parents to complete some simple work whilst their children were within the school. Parents need to remain with their children (mainly due to the travelling), however offering parents some simple work has been identified as enabling families to prioritise attending the school as well as earning a small amount of additional monies.
- addressing delegates
- support from the police
- the SAAHAS model
The purpose of SAAHAS is ,as the posters suggest, to ‘reach out’ to those members of their local communities who have an intellectual disability and their families. There are however a number of difficulties that this program faces, first of all it’s being managed by the state police and therefore the motivations of the officers involved have been questioned by local village leaders, villagers and families. However, the compassion and commitment to this project from DSP Kumar all the way down to his officers has appeared to shine through and local constables are visiting villages and being able to discuss SAAHAS. To ensure that this process continues, grows and supports “grassroots” approaches to the fundamental aspects of SAAHAS then I was able to access and speak with trainee constables at one of the police training academies. In relation to the continued success of SAAHAS and relevant to practice within the UK is the fact that training around the needs of people with an intellectual disability can offer better outcomes. Nurse education requires students to know something about the needs of people with an intellectual disability, however this is now being shared with other professional groups such as teachers, social workers, doctors, and there are examples of training programs being added to police service training so that of officers have an idea about how to support people with an intellectual disability. In the UK this has been seen as a great addition in relation to disability related crime, as well as identifying individuals with an intellectual disability who may commit offences. This means that police officers can have some knowledge of the needs of this vulnerable group, they can engage with families, individuals and wider communities, thus supporting their crime prevention activities as well as being able to respond more successfully with people who have an intellectual disability. SAAHAS is a police initiative, the police in India are a respected institution; enabling them to connect can only be a good thing and in my view supports the role of the nurse especially the learning disability nurse.
Conclusion;
My trip ends with a number of quotes in my head, most of them I have used in my presentations and I wanted to shared them to give what I believe is some insight into my experience;
“Carefully watch your thoughts, for they become your words. Manage and watch your words, for they will become your actions. Consider and judge your actions, for they have become your habits. Acknowledge and watch your habits, for they shall become your values. Understand and embrace your values, for they become your destiny.”
“Be the change you wish to see in the world”
Mahatma Ghandi (Date Unknown)
This organization are seeking to break down the barriers that are faced by people with an intellectual disability within their community. Uttar Pradesh is a vast, beautiful and clearly complex environment where services don’t always know or seek out the most vulnerable within their community. SAAHAS is seeking to change that, they truly wish to make the “Invisible – Visible”, and I am privileged to have been witness to some of their activities.
2011 Nurses League Travel Award,
The winners Becci Sloan and Abigail Hosier were invited to the Annual Meeting and gave a powerpoint presentation about their visit to Hyderabad in South India.
Becci and Abigail work in the Tropical and Infectious Diseases Unit at the Royal Liverpool Hospital. They currently focus on caring for individuals with HIV and Hepatitis and the travel award assisted in enabling them to visit and work with LEPRA in India.
We learned about the work of LEPRA in India and the immense problems faced.
Since returning to Liverpool, Becci and Abigail have created an information pack for newly diagnosed HIV Positive patients.
Many thanks to Becci and Abigail for such an interesting and informative presentation.
Visit to LEPRA Hyderabad Services and Projects
(Andhra Pradesh, South India) 2013
I applied for the travel award with my colleague Abigail Hosier who I studied with at the University of Liverpool. We both share a passion for working in resource poor settings overseas and following graduating in 2005 worked together on the Tropical and Infectious Diseases Unit (TIDU) at the Royal Liverpool University Hospital. In recent years we have focussed on caring for individuals with HIV and Hepatitis; both in research and in specialist nursing.
Over the years working in this area we have established a growing awareness of the need and importance of good quality holistic care. This is very apparent within the context of the care of the newly diagnosed HIV positive patient. The TIDU department provides a high quality service and we have an established multi-disciplinary team which includes specialist nurses, counsellors, community HIV nurses and medical staff. Over recent years we have spent time with patients and gained a greater understanding of the experience of being diagnosed with HIV. We felt that whilst there were many areas of excellent practice, that there were also areas of improvement in relation to the support of newly diagnosed individuals.
The importance of providing holistic care is highlighted in the range of different patients we care for. Many have little or no support, which is often made worse by the nature of the diagnosis and the stigma surrounding HIV. A lot of people tell very few people about their HIV positive status and therefore often feel isolated and alone in coping with their diagnosis.
In recent months we spoke with patients and staff about what they felt improvements could be made in the care of newly diagnosed patients in our department. The main issues that arose through these discussions were surrounding spiritual, mental and social care. The diversity of these issues is vast and we endeavour to always support our patients in all these areas, so we began to wonder how we could improve our service.
The opportunity of working with LEPRA in India was excellent as we were very keen to gain an insight into how holistic care is provided for patients there suffering from conditions with immense social stigma. As emphasised in the mission statement of LEPRA;
‘LEPRA – health in action; is a health and development organisation working to restore health, hope and dignity to people affected by leprosy, tuberculosis, malaria, HIV/AIDS, blindness and other health conditions exacerbated by stigma and social discrimination’.
As resources are more limited in Hyderabad and up to date medications are not available to most people living with HIV, more focus is put on holistic care of patients. We hoped to be inspired by how they managed their patients in such a resource poor setting.
Abigail and I are both keen to develop our careers through personal and professional development and held the belief that this award would be an excellent way to do this. We are enthusiastic about enhancing our knowledge within our area of expertise and are passionate about working overseas and would love to work in a developing country within a nursing capacity in the future.
Our aims in applying for the travel award were:
To enhance our knowledge and gain insight into the treatment, management of nursing/medical care and the outcomes for people living with HIV in India.
To work along side staff working with people with HIV in the region, observing practice and implementation of care.
To be able to compare my experiences and the information we obtain, with treatment, care management and outcomes of the patients we care for here in the Infectious Diseases Unit at the Royal Liverpool Hospital.
During our time with LEPRA in Hyderabad we were overwhelmed by the care and attention the LEPRA staff gave to both us and to the people they cared for. We were very humbled by the compassion that was shown by each member of staff. One event that particularly impressed us was a shoe distribution ceremony:
Many people with leprosy have been diagnosed late in the disease progression, by which time they have suffered severe peripheral damage, particularly in their feet. Many have very deformities and lost toes after suffering burn injuries, pressure sores and ulcers. Wearing shoes becomes very difficult and can often exacerbate the problem, causing new sores.
LEPRA individually fitted tailor made new shoes for about 100 people suffering from leprosy and held a ceremony for each person to be presented with their new shoes. Each person came up one by one and was overjoyed to be presented with their shoes and with a first aid kit. They were then delighted to be provided with lunch afterwards.
We loved being part of this event as it demonstrated to us an innovative way to show compassion and support to individuals suffering from an isolating and stigmatising condition. We wanted to capture something of this as an inspiration in our department. However, as all newly diagnosed HIV positive patients are individual, ‘holistic support’ means something entirely different to each person. The example of holistic care in India would not transfer into our culture so exactly.
We therefore decided to enhance the information newly diagnosed patients are provided with, by creating a ‘Newly Diagnosed HIV Positive Information Pack’ in order to signpost them to various places where support is available. We understood that everyone’s needs are different and that people needed to receive support in different ways. Compiling all the services we offer and support that is available around the city into one leaflet allows a patient to easily choose the type of support they would like to access.
In Hyderabad there is a high proportion of sex workers, who due to the attitudes of society are often marginalised and isolated from local communities. In order to encourage them to access healthcare services, there needed to be appropriate ways of displaying acceptance and non-judgemental care. One of the ways in which this was achieved was through the facilitation of support groups specifically designed to meet the holistic needs of the women.
The service we offer to our HIV positive patients is also one of acceptance and non-judgemental care. However finding new ways to support patients and being inspired by other service providers can be beneficial. We therefore are considering opening a support group for our HIV positive patients. We recognise that this would not appeal to every individual, which emphasises the importance of an information pack including information on all the support options available.
We have planned a presentation in the hospital in conjunction with the hospital Arts Lead. This will be an opportunity for us to tell patients, staff and the general public about our experiences in India. We hope that our presentation will inspire people and give them a fresh insight and a wider perspective of healthcare.
We have discussed these plans with the Lead Consultant and other members of the MDT of the TIDU and they are keen for this to go ahead as ideas like these, would benefit the patients in our care and help staff to be well equipped to resource patients.
Our trip to work with LEPRA was an incredible experience and has increased our knowledge and motivation in the holistic support of HIV positive patients in our care.
We are also excited by the links that we have formed between the TIDU and LEPRA and will be keen to maintain the good professional relationship that we have established during this trip.
We would be keen to encourage fellow staff on the benefits of seeing firsthand the practices of non government organisations, in resource poor settings and how this can both, motivate, inspire and facilitate personal growth as a professional. Our presentation and display will be a good way of encouraging this.
Most of all we are looking forward to hearing the feedback and comments of the patients utilising the additions to the current service.
We would like to take this opportunity to extend our sincere thanks to the Royal Infirmary Nurses League for the travel award. We believe the experience has been motivating, challenging and rewarding and we are very grateful for the financial investment we received.
Becci Sloane
Abigail Hosier
Tropical and Infectious Diseases Unit
Royal Liverpool University Hospital Trust
TRAVEL AWARD to Christine O Connor 2011
Following a successful application for the Royal Infirmary Nurses’ League Travel Award, I was able to visit Melbourne, Australia, to view how they undertake Infection Prevention and Control particularly relating to multidrug resistant organisms, outbreak management and education. I spent a total of two weeks visiting two large Health Care settings, Southern Health Care and Alfred Health in Melbourne. I also had the opportunity to visit the National Surveillance Centre.
My first visit was to the Southern Health Group which is the largest public health service in Victoria, covering 40 locations. Services provided include acute teaching, research and community hospitals, mental health and community outreach services. I visited Monash Hospital and Dandenong Hospital within the Southern Health Group, both of which are teaching and referral hospitals.
The other major healthcare setting I visited was The Alfred, which is a major tertiary referral teaching hospital. Specialist services include trauma services, emergency and intensive care, heart and lung transplantation and burns. Within the healthcare group I was also able to visit 2 other hospitals Caulfield, which specialises in community services, rehabilitation and aged care and Sandringham, specialising in maternity and surgical services.
My first port of call was to Monash Hospital and feeling a bit jet lagged I was fortunate to attend one of the fortnightly meetings with all the ‘Infection Prevention and Control Team’ (IPCT) from all the locations. Agenda items discussed included rates of infections ‘vancomycin resistant enterococcus’ (VRE), ‘Clostridium difficile toxin’ (CDT), occupational exposure to needle stick injuries, Hand Hygiene programme, support services and Newsletter. It was very interesting to hear that a new strain of CDT 064 had emerged which is predominately in Australia.
The State of Victoria has a very well established mandatory hand hygiene surveillance programme, whereby every hospital submits quarterly ‘hand hygiene observation data’ to the surveillance centre. The audits are undertaken by the IPCT, 50 observations per ward are required from a maximum of seven ward areas depending on the size of the hospital. These are collected by the surveillance centre and hospitals are compared to the national benchmark. The Victorian Department of Health has set a target of 70% compliance. In the United Kingdom (UK) each Trust will undertake their own hand hygiene audits, it is not mandatory by the Department of Health. There is no national bench marking currently, but this may come in the future.
I had the opportunity to participate in their internal ‘Safety Quality Audits’ within the Southern Health Group. This involved visiting several clinical areas with a team of specialist staff including the Director of Nursing, Senior Nurses, Estates and cleaning personnel. Some of the clinical areas were in the process of being renovated; oneparticular ward wasactually circular, reminding me of a picture I once saw of the old Royal Infirmary. They appeared to experience similar problems to the UK with limited storage facilities, some areas required more hand wash basins, although upgrade of areas were in the process of being addressed. All healthcare setting are accredited and have to comply with specific standards, one of which is infection control, similar to the UK.
Outbreaks
Both hospital groups had experienced outbreaks of Norovirus, however Alfred Health had been particularly affected last year, with most of the ward areas being affected at some point. The outbreak lasted for several weeks putting considerable pressure on the resources and the running of the hospital. One of the problems which was highlighted and potentially could have prolonged the outbreak was incorrect cleaning methods, for they used a two stage cleaning process with detergent followed by sodium hypochlorite. It was thought that in some areas, that the first stage of cleaning with detergent was not being undertaken correctly. It was good to share experiences, with the management being very similar to that in the UK, however they used an electronic data base that assisted them in patient management and movements. This was highlighted using the ‘RAG’ rated system (Red Amber Green), to make it visually easier to identify which patients are symptomatic, those at risk of becoming symptomatic and those who have recovered from norovirus. This seemed to work very effectively’ although appeared to be time consuming with data entering. This would be worth investigating to adapt a similar approach at the Royal Liverpool University Hospital (RLH)
Influenza
With influenza being a potential threat each winter causing some deaths, it was amazing to hear what new research was being undertaken with their well established surveillance system on Severe Respiratory Illness known as the ‘FLuCAN’. From 2012 the surveillance system will be increased to cover 15 sites across Australia. Current surveillance systems are designed to estimate influenza activity in the community. It is hoped that this new research will fill the gap in surveillance between community and hospitals. The aims are to: collect real time sentinel surveillance on patients that require hospitalization for influenza; clinical and laboratory information on ‘laboratory confirmed’ influenza patients, to determine the burden of disease requiring hospitalization; estimate the effectiveness of the influenza vaccine and vaccine coverage from patients with community acquired pneumonia prior to the onset of the influenza season. I was surprised to find that ‘face fit’ testing of respiratory masks, was not undertaken before being able to nurse patients with severe respiratory illness, although ‘face fit’ testing was not undertaken, the healthcare workers on the Infectious Diseases Unit checked their masks by looking into a mirror. This enabled the healthcare worker to adjust their masks to ensure a sufficient seal had been created before entering an infected room.
In the Southern Health Group hospitals, staff vaccination was undertaken by the IPCT including measles, mumps, rubella and seasonal flu. This was not the common practice in all hospitals in Australia, in some it is the responsibility of the Occupational Health Department as in the UK, however the Royal Liverpool IPCT, does assist in undertaking Flu Vaccination.
All the teams were very interested in the DVD which was made at the Royal Liverpool Hospital ‘Killer Bug’ to promote vaccination of healthcare workers. The Surveillance Centre Team asked if they could enter this into a national competition to promote flu vaccinations.
Education
I had the opportunity to attend and participate in the IPC nurses’ link group meeting, as I was very interested in their role. The role was very similar to that in the UK, to liaise with the ward team, however their audit programme was very limited compared to the UK, only undertaking a full environmental audit annually.
In the Southern Health Group Hospitals, the link nurses had an excellent 3 day educational induction programme, which included topics on microbiology, history of Infection control and decontamination. On completion of the programme, an examination was undertaken to access their knowledge and understanding, only on the successful passing of this examination, were the staff able to undertake the role of Infection Control Liaison Nurse.
It was a common occurrence that the IPCT participated in the induction training of newly appointed staff. However I was very surprised to find that there did not appear to be a regular ongoing mandatory training system, instead appearing to be ad-hoc, within the clinical areas. I found that the IPCT in both healthcare setting were larger than what we had at the RLH. They had a self regulatory process known as ‘credentialing’ which all IPC practitioners had to undertake, to determine and acknowledge that an individual has demonstrated the competences of the specialist role.
Surveillance
Having the opportunity to visit Victoria Healthcare Associated Infection Surveillance System was excellent. I met up with their small team and discussed the type of surveillance data which they collected. I presented a power point presentation of the work which is undertaken by the Health Protection Agency and NHS Trusts in the UK, on targets and data collection. The State of Victoria collected data on colorectal, surgical site surveillance including cardiac, orthopaedic, in hip and knee surgery, caesarean section, spinal surgery and hand hygiene. This is similar to the UK however data is also collected on central lines, to determine the rates of bacteraemia (blood stream infection) by calculating the number of days a central line has been in situ. It was very interesting to hear that a trial was being undertaken on the monitoring and documentation of insertion practices for central lines in Intensive Care Units, with 5 large hospitals being involved. This is similar to the ‘Saving Lives High Impact Interventions’ that are widely used in Hospital Trusts. However within the UK, this is not mandatory and only collative in individual Trusts. It will be interesting to see how this develops.
Intensive Care central line associated bloods stream infection surveillance is undertaken nationally, data being collected from most Australian states which allow local and national benchmarking. The aim is to improve patient safety by reducing blood stream infections in central lines. Surveillance data collection was introduced in 2010, however definitions were variable. This has now been standardised and a national database and reporting system isin operation whereby State based surveillance centres will forward data to the national database. In the UK this data collection is not mandatory, with wide variations between Hospital Trusts in how, or if, this data is collected and how this is reported. At the RLH the data which is collected is fragmented and therefore it would be worthwhile to take this forward.
Resistant organisms
Although both health settings had experience with Methicillin Resistant Staphylococcus aureus (MRSA) it was only Alfred Health Care that appeared to have experience with some of the resistant gram negative organism. Going back several years to 2004 they had experienced one or two cases of Acinetorbacter in their Intensive care unit. Acinetobacter is a Gram-negative bacterium that is readily found throughout the environment including drinking and surface waters, soil, sewage and various types of foods, this then has the potential to contaminate the environment. While Acinetobacter poses few risks to healthy individuals, a few species, particularly Acinetobacter baumanni, can cause serious infections – mainly in very ill hospital patients. The most common Acinetobacter infections include pneumonia, bacteraemia (blood stream infection), wound infections, and urinary tract infections. `Hospital-adapted` strains of Acinetobacter are sometimes resistant to antibiotics and are increasingly difficult to treat. Acinetobacter can live on the skin and may survive in the environment for several days. Transmission can be reduced by careful attention to infection control procedures such as hand hygiene, environmental cleaning and disposal of exposed medical equipment after patient discharge.
The number of Acinetobacter cases appeared to increase following the Bali bombing in 2005 where several burns patients were airlift to the hospital for specialist treatment. Overtime different interventions had been introduced on the Intensive Care Unit (ITU) such as enhanced cleaning, wearing of gowns/ gloves for direct patient contact and Antibiotic Stewardship. Environmental sampling, although the cases did not appear to be connected the source was unknown and it wasn’t until the ITU moved into a new area that the source was eradicated. Their ITU now is a modern 45 bedded purpose built unit with direct access to the helicopter pad. One of the interventions that were imposed was to stop the use of the antibiotic meropenem which is from the group of antibiotics known as the carbopenamase, which is widely used in the UK to treat serious infections. Since the introduction of electronic prescribing this has vastly improved antibiotic stewardship, optimising antimicrobial use in order to improve patient outcomes, ensure cost-effective therapy and reduce antimicrobial resistance.
In the UK we are starting to see resistance to this classification of antibiotics; however this appears to be a radical approach. Other Interventions that I was particularly interested in were the use of chlorhexidine wash cloths which are used daily on all ITU patients. Also the use of chlorhexidine biopatch dressing used on central venous lines insertion sites to reduce colonisation and prevent infection. The RLH is now exploring the possibility of using these.
Both healthcare settings over the last six years had seen a substantial decline in MRSA while VRE, (vancomycin resistant enterococcus) rates remain steady.Patients can be colonisedwith VRE or some may develop a severe infection. At present there is no treatment which can reduce the ‘carriage’ of VRE. Alfred Health has always adopted a ‘once VRE, always VRE’ policy, as there is no expert agreement on how long people carry VRE once they show the signs of contact, or the best approach to this problem. All VRE patients are placed in isolation in a single room to limit their movement around the ward and reduce the risk of the infection spreading to other patients. Research is being undertaken by screening patients who have been identified as VRE carriers over the last ten years, with the aim to find out how long people carry VRE for and that the most appropriate care is provided.
Alfred Health had made a DVD called Glen’s Story, which was hard hitting, focussing on a patient’s experience after contracting MRSA bacteraemia. He was actually a Doctor working at the hospital and his fiancée was an IPC Nurse. Both these can be viewed on ‘You Tube’.
Infection Prevention and Control Practices
Whilst visiting some of the ward areas, major differences that I observed, were staff using disposable gowns and gloves when caring for infected patients, where as in the UK we tend to use disposable plastic aprons and gloves. If there was a lack of isolation facilities it was their policy to mark on the floor with wide sticky tape, a boundary around the patient’s bed area to identify the patient zone, to enable IPC precautions to be undertaken.
Isolation notices were very different between the two heath care settings, one using different colour notices and illustrations to get the message across, whereby the other had about 12 different signs, all coloured yellow, with a slight variation on the message which were quite worded, however these where in the process of being reviewed. What did interest me was that nationally, the Australian Infection Control Association, was considering the feasibility to have generic isolation precautions posters across the country.
The Alfred had recently undertaken a patient improvement safety project to reduce urinary catheter infections. This used a light hearted approach to increase patient and staff awareness and improve documentation of catheter management to minimise infection, involving designing and implementing posters, patient information leaflets and a computer education programme. I thought the posters that had been produced were very innovative with a picture of a kangaroo and the caption ‘Tie me catheter down’.
At Southern Health they employed a marketing person for 1 day a week, to develop IPC posters, signage, promote campaigns i.e. hand hygiene, which were very innovative.
Towards the end of my trip I managed to have a few days to relax and take in some of the sights of Melbourne visiting the newly built AAMI stadium to watch Melbourne Storm, Rugby League Club, sightseeing, viewing the wine region and seeing koalas and kangaroos, which were amazing and of course fitting in time for some retail therapy (shopping).
Conclusion
Visiting Australia was a fantastic opportunity and experience, giving me the opportunity to network with colleagues, who were extremely helpful, willing to share experiences,enthusiastic and made me feel very welcome. Even though I had specific objectives to concentrate on, sometimes it was difficult not to get side tracked, for IPC is such a vast area and when visiting clinical areas I was so enthusiastic that I wanted to see as much as possible. I felt that I had gained so much more than I had originally planned; my aim now would be to implement some of the findings that would be beneficial to the patients and staff at the RLH.
Acknowledgements
I would like to take this opportunity to thank Elizabeth Gillespie, Southern Health, Dr Anne Bull VICNISS and Sue McClelland. Alfred Health, for accommodating me and being excellent hosts. Thanks also go to Marie Dewhurst my Manager and Diane Wake, Director of Nursing, for enabling me to take this fantastic opportunity.
Christine O’Connor
Nurse Specialist in Infection Prevention and Control.
Royal Liverpool University Hospital NHS Trust.
Christine O`Connor, Nurse Specialist in Infection Control at the RLBUHT, is joint winner of this years LRI Nurses` League Travel Award. Further details about this years winners will appear in the journal.
Love the frilly, Christine
Photo – Student Nurse Claire Barstow and Christine manning the Infection Control stand at the recent Nurses` Day exhibition at the Royal Liverpool Hospital